Lifting up your little ones, sneezing, or laughing with friends, we've all had those moments of...oops!
Urinary incontinence is extremely common and affects up to one in two women (30-50 per cent). Perhaps you've heard of stress incontinence and urge incontinence. But what exactly is it? Keep reading below for a quick rundown on a condition that affects millions of people and discover the best continence aids today!

What is Urinary Incontinence?
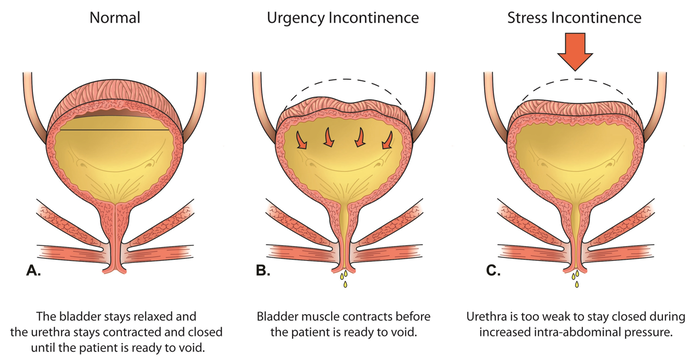
Basically, it involves the involuntary loss of urine. There are different types of incontinence with the most common being stress incontinence and urge incontinence.

Stress incontinence
Stress incontinence is triggered by pressure on your abdomen, such as when you exercise, laugh, sneeze, lift a heavy object or bend over. This condition is more common in women; however, some men may develop it after prostate surgery.
Urge incontinence
On the other hand, as for urge incontinence - the clue is in the name! It refers to when you have an overactive bladder, resulting in an intense urge to go to the toilet and sometimes you leak urine before you get there.
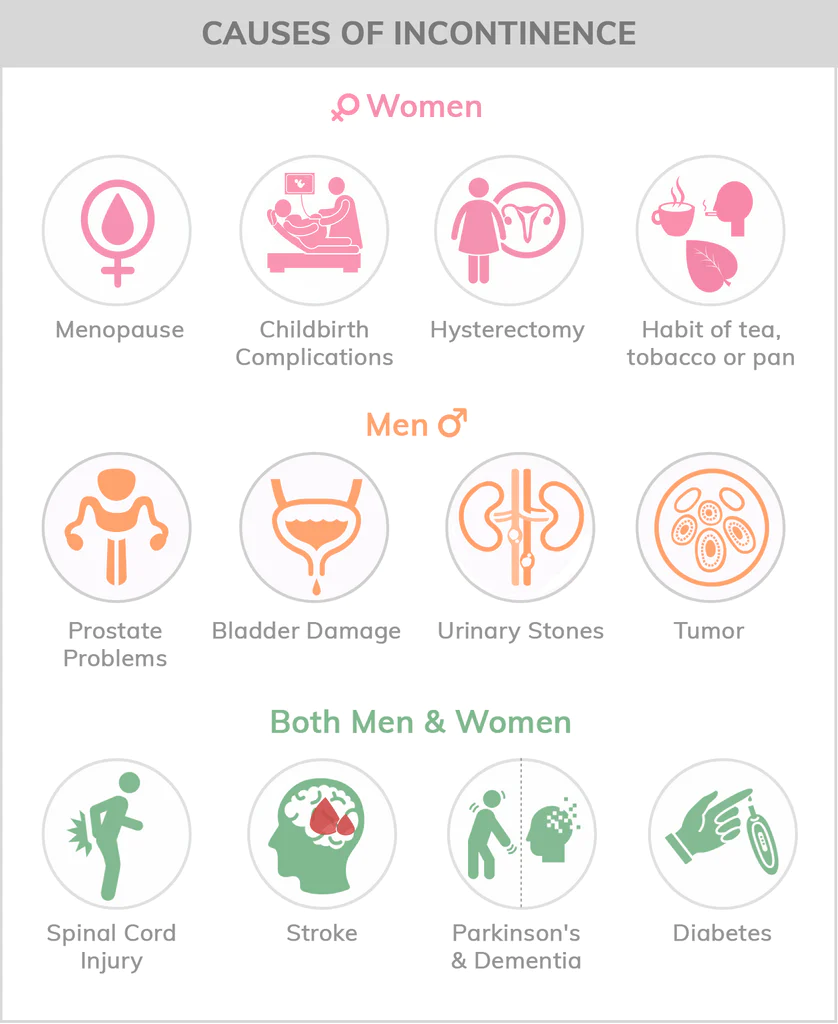
What causes stress & urge incontinence?
Most women experience incontinence due to childbirth and/or menopause. During pregnancy, strain from supporting a growing baby and changes in hormones weaken your pelvic floor muscles. For example, picture your pelvic floor as a "hammock" of muscles, ligaments, and tissues that support your bladder. These bladder muscles further weaken during labour from pushing, and again after menopause when your body produces less estrogen.

Additionally, other risk factors include:
- Constipation
- Obesity
- Older adults (over 65 years)
- Dementia
- Nerve damage impeding your brain from sending messages to your bladder (like a stroke, Multiple Sclerosis, or Parkinson's disease)
- Have a history of poor bladder habits (e.g. going to the toilet just in case)
- Have a prolapse where your bladder, uterus or bowel has 'dropped down into your vagina and places pressure on your bladder
Meanwhile, sometimes incontinence is only temporary and is caused by:
- Side effects from certain medications, such as diuretics (water pills). They are used to treat heart failure, hypertension, some kidney diseases, and liver cirrhosis. Your symptoms will often go away once you stop taking the medication
- Excessive caffeine consumption
- Infections, such as urinary tract infections may cause incontinence for a short period of time
How is Incontinence Diagnosed?
To be sure, make an appointment with a health professional. Prepare to be asked a bunch of questions so come ready. Tips and advice to prepare for your appointment.
This will help you answer any questions that your doctor may have, such as:
- How often do you empty your bladder?
- How and when do you leak urine?
- How much urine do you leak?
- When do your symptoms start?
- Are you on any medication/s?
- If you have been pregnant how was your labour/delivery experience?

Your doctor or nurse will then perform a physical exam to look for signs of any health problems and may also conduct further tests, including:
- Urine test. The doctor will ask for a urine specimen which will be sent to the lab to check for infection or other causes of incontinence
- Ultrasound. Your doctor will look for anything unusual in your bladder, kidneys, and urethra
- Bladder stress test. During this test, your doctor will ask you to cough or push as if you are in labour and check for any loss of urine
- Cystoscopy. Your doctor will insert a thin tube with a tiny camera inside your bladder and urethra to look for damaged tissue
- Urodynamics. Your doctor will insert a thin tube into your bladder and fill it up with water to see how much liquid it can hold. This is designed to test your bladder control and measure your bladder pressure

Once you’ve gotten your diagnosis, your healthcare professional can direct you to treatment options that will improve your quality of life!
Urinary incontinence treatment
From first-line treatments to advanced therapies and continence aids, there are various treatment options for all types of urinary incontinence available now!
First-line urinary incontinence treatment
- Lifestyle changes, e.g. losing weight, bladder training
- Behavioural treatments
- Pelvic floor exercises, recommended by healthcare professionals as an initial solution for stress incontinence
- Medication
- Mechanical treatments
Advanced treatment
Continence aids
Apart from pads and underwear, you can also manage your symptoms with seat cushions and supports. For instance, you'll find there are reliable seat cushions, pads and wedges available now if you suffer from incontinence.
Shop a wide range of continence aids, used in homes, nursing facilities, and hospitals at the Therapeutic Pillow. Here, it's our mission to provide comfort and peace of mind to those affected by incontinence. Discover cushions, such as the Keyhole Comfort Cushion and Ring Latex Cushion featuring cut-out areas to provide coccyx pressure relief. They are perfect for those that are postpartum or post-surgery.
Other continence aids that are designed to provide support and stability while sitting, include our Angled Pommel Cushion, Diffuser Pommel Cushion or Bed Seat Cushion.
Why you'll love our incontinence cushions
- Proudly Australian-made and owned
- Features hospital-grade moisture and bacteria-resistant SteriPlus cover - can be wiped down or removed and is machine washable
- Designed by healthcare professionals
Lastly, there are a number of online support groups where you can share your experiences with others who are in the same position. In addition, you can find a list of local incontinence communities.
Of course, there is lots more information on www.supportincontinence.org: go and explore!
Do you want to learn more? Read our Frequently Asked Questions for...
Creating a supportive environment involves both emotional and practical adjustments. Use empathetic communication to understand their needs and concerns. Practically, arrange furniture for easy access, ensure bathrooms are accessible, and utilize protective products to maintain dignity and cleanliness.
 0
0 0
0Diet plays a significant role in managing incontinence. Certain foods and beverages, like caffeine, alcohol, and acidic foods, can irritate the bladder. A high-fiber diet helps maintain regular bowel movements, reducing incontinence incidents. Monitoring fluid intake is also crucial.
 0
0 0
0Establishing a consistent toileting schedule can greatly assist in managing incontinence. Incorporating regular skin care routines to prevent irritation and maintaining a balanced diet can also contribute to better incontinence management.
 0
0 0
0Bladder incontinence, also known as urinary incontinence, is a condition characterized by the involuntary loss of urine from the bladder. It can be caused by various factors, including weakened pelvic floor muscles (stress incontinence), sudden and intense urges to urinate (urge incontinence), incomplete bladder emptying (overflow incontinence), physical or mental impairments that hinder reaching the toilet in time (functional incontinence), and sometimes a combination of these factors (mixed incontinence). Bladder incontinence can affect individuals of all ages and genders and can have physical, emotional, and social implications. Understanding its types and underlying causes is essential for effective management and treatment.
 0
0 0
0Incontinence is a condition that affects the control of bladder or bowel movements. It can cause unintentional leakage of urine or feces, leading to embarrassing situations and affecting a person's quality of life. Incontinence can occur due to various reasons, such as weakened pelvic floor muscles, nerve damage, hormonal changes, or certain medical conditions. It is more common in older adults, women who have given birth, and individuals with certain health issues. However, it is important to note that incontinence is not a normal part of aging and can be managed or treated with the help of healthcare professionals.
 0
0 0
0Previous
Next
Nursing pillows are safe when used as directed, supporting the baby in a stable and comfortable position during feeding. Always supervise your baby and follow safety guidelines to prevent risks.
 0
0 0
0Some individuals find relief with dietary supplements such as black cohosh, vitamin E, and soy products, which are thought to have estrogen-like effects. However, it's important to consult with a healthcare provider before starting any supplements, as they can interact with other medications.
 0
0 0
0Non-hormonal therapies for managing hot flushes include lifestyle adjustments, cognitive-behavioural therapy, and certain medications like antidepressants. Acupuncture has also been suggested as a potential treatment, though research results are mixed.
 0
0 0
0Yes, the Diffuser Cushion comes in a bariatric size designed for larger body frames, providing enhanced support and pressure relief to accommodate the unique needs of heavier individuals.
 0
0 0
0Antihistamines, decongestants, and nasal corticosteroids are commonly used to alleviate allergy symptoms and improve sleep quality. However, it's essential to consult with a healthcare professional before starting any medication regimen.
 0
0 0
0